心肌病 心律失常 肌病 多基因突变
男童心肌病,特别是心室致密化不全,存在心律失常,合并有肌病、中性粒细胞减少、3-甲基戊烯二酸尿症,需要重视心肌病基因筛查。有研究表明,男童心肌病患儿中,5%为Barth综合征。越来越多的小儿心内科医生开始认识该疾病。今天的阅读笔记是多基因突变的Barth综合征。
存在三个基因突变的Barth综合征
Barth syndrome associated with triple mutation
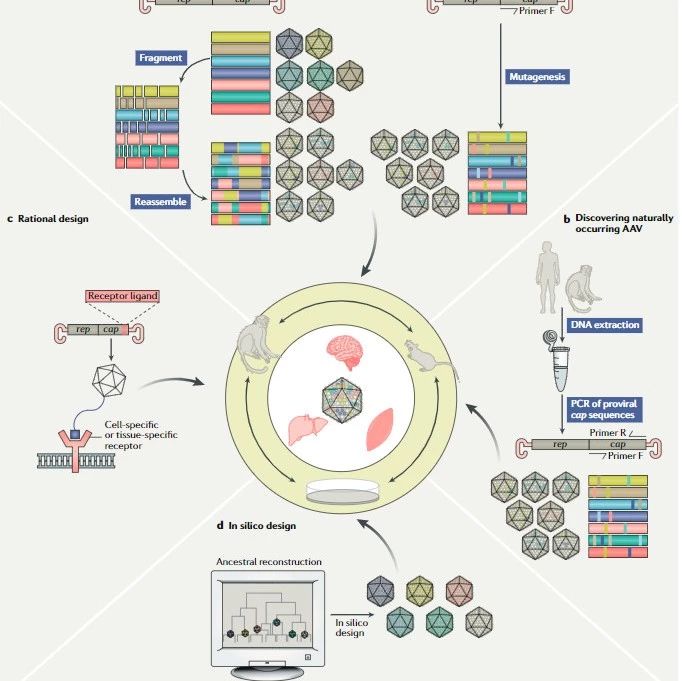
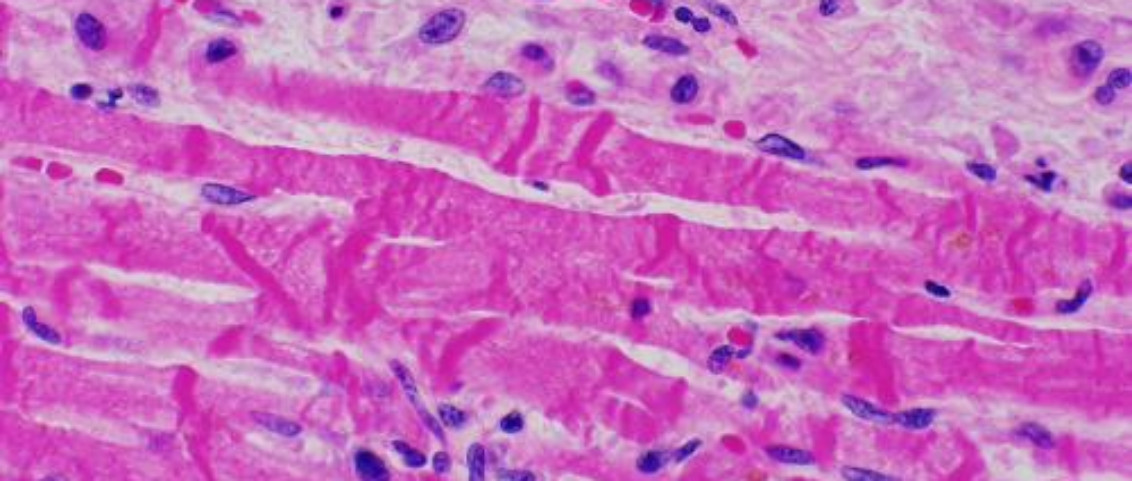
患儿,足月男婴,2582g,其母33岁,健康。怀孕和分娩都很顺利。出生后3小时,由于呼吸困难、混合性呼吸代谢性酸中毒以及经胸超声心动图显示左心室(LV)功能下降,被转运到目前的医院。患儿心率快,血氧饱和度低(86%),X线胸片显示心胸比为66%,表现为心源性疾病。超声心动图显示左心室功能整体下降,射血分数为25%,舒张时左心室增大(比正常大158%)。左心室是高度和广泛小梁化(图1b)。各节段心肌的非致密化与致密化之比均大于2.0。心电图显示II、III、AVF和V4-6导联的左室肥大和ST段压低。诊断为急性心力衰竭的左心室致密化不全和扩张型心肌病。气管插管,使用卡维地洛与正性肌力药物。尽管患儿在5个月大时出院,但他反复出现慢性心力衰竭、室性心律失常和肌肉减少的急性加重。在28个月大的时候,体重为3.3公斤(低于7.8标准差)。没有中性粒细胞减少或单核细胞增多症,但在6个月大时出现了3-甲基戊二酸检测阳性(+4.1 sd)。
A full-term male infant weighing 2,582 g was born to a 33-year-old healthy mother. Both pregnancy and delivery were uneventful. Three hours after birth, he was transferred to the present hospital because of dyspnea, mixed respiratory-metabolic acidosis, and decreased left ventricle (LV) function on transthoracic echocardiography. Gallop rhythm, low oxygen saturation (86%), and auxocardia with cardiothoracic ratio 66% on chest X-ray were noted. Echocardiogra-phy showed globally decreased LV function with an ejection fraction of 25%, and enlarged LV dimension in diastole (158% of normal). The LV was highly and globally trabeculated (Fig. 1b). The ratio of non-compacted to compacted myocardium was >2.0 in all the segments. Electrocardiography showed LV hypertrophy and depressed ST segment in leads II, III, aVF, and V4–6. He was diagnosed with acute heart failure from LV non-compaction (LVNC) and dilated cardiomyopathy (DCM). He was intubated, and carvedilol was also later given along with the inotropic drugs. Although he was discharged at the age of 5 months, he had repeated acute aggravation of chronic heart failure, ventricular tachyarrhythmia, and reduced muscle mass. At 28 months of age, he had already lost weight and weighed 3.3 kg ( 7.8 SD). He did not have neutropenia nor monocytosis but developed 3-methylglutaconic aciduria at 6 months of age (3-methylglu-taconic acid level, +4.1 SD).
关于家族史,他的哥哥出生后17小时突然夭折,他的外祖母经历了两次自然流产(图1a)。遗传分析得到了参与研究机构医学研究伦理委员会的批准,并获得了婴儿父母的书面知情同意。心肌病相关基因的靶向测序证实,患者在tafazzin(TAZ)、琥珀酸脱氢酶复合物黄素蛋白亚基A(SDHA)和a-反转录病毒(DTNA)有变异。这些变体在TAZ的外显子6,c.469c>t(p.leu157phe)中被鉴定;SDHA的外显子10,c.1351_1355delcgcct(p.arg451 fs)和DTNA的外显子19,c.1763g>a(p.ser588asn;图1d-f)中被鉴定。在进一步分析中,这些罕见的变异可能是致病的。经TAZ基因分析,诊断为Barth综合征。
With regard to family history, his elder brother had died suddenly 17 h after birth, and his maternal grandmother had experienced two spontaneous abortions (Fig. 1a). The genetic analysis was approved by the Medical Research Ethics Committees in the institutions that participated, and written informed consent was obtained from infant’s parents. Targeted sequencing of the cardiomyopathy-associated genes confirmed that the patient had novel rare variants in tafazzin (TAZ), succinate dehydrogenase complex flavoprotein subunit A (SDHA), and a-dystrobrevin (DTNA). These variants were identified in exon 6 of TAZ, c.469C>T (p.Leu157Phe); exon 10 of SDHA, c.1351_1355delCGCCT (p. Arg451 fs); and exon 19 of DTNA, c.1763G>A (p.Ser588Asn; Fig. 1d–f). On in silico analysis these rare variants may be disease causing. On genetic analysis of TAZ, the patient was diagnosed with Barth syndrome.
通过对患者父母基因的进一步测序分析,发现他的母亲有相同的TAZ突变,而他的父亲有SDHA和DTNA突变,这些突变都是半合子或杂合子。先证者被证实有母系和父系的突变,因此被认为是三重半合子或杂合子。他的父母和活着的兄弟姐妹没有心肌病的临床证据,但他的父亲被怀疑有心功能正常的左室肥大(图1c)。
On further sequencing analyses of genes from the patient’s parents, his mother was found to have the same TAZ mutation, while his father had the SDHA and DTNA mutations, all of which were hemi- or heterozygous in nature. The proband was confirmed to have both maternal and paternal mutations and was therefore considered as triple hemi- or heterozygote. His parents and living siblings had no clinical evidence of cardiomyopathy, but his father was suspected to have LVNC with normal cardiac function (Fig. 1c).
图1
(a)家族系谱:父母的第二个出生的男婴在出生后17小时突然死亡,他的外祖母有两次自然流产(棕色箭头)。(b,c)先证者及其父亲的经胸超声心动图(b)显示左心室(LV)顶点和游离壁增厚的长轴视图,表明左心室致密化不全(LVNC)。(c)短轴视图显示左室游离壁增厚,表明左室致密化不全。(d–f)来自先证者的Sanger测序数据,表明(d)母体半合子tafazzin(TAZ)突变和(e,f)父系杂合子(e)琥珀酸脱氢酶复合物flavoprotein亚基A(SDHA)和(f)a-反转录病毒(DTNA)突变。
Fig. 1 (a) Pedigree. The second-born male infant of the parents had suddenly died 17 h after birth, and his maternal grandmother had two spontaneous abortions (brown arrows). (b,c) Transthoracic echocardiography of the (b) proband and (c) his father. (b) Long axial view demonstrating thickening of the apex and free wall of the left ventricle (LV), suggesting LV non-compaction (LVNC). (c) Short axial view showing thickening of free wall of the LV, suggesting LVNC. (d–f) Sanger sequencing data from the proband, indicating a (d) maternal hemizygous tafazzin (TAZ) mutation and (e,f) paternal heterozygous (e) succinate dehydrogenase complex flavoprotein subunit A (SDHA) and (f) a-dystrobrevin (DTNA) mutations.
讨论
这是由三重突变引起的左心室致密化不全报告,与Barth综合征有关。Barth综合征是一种X连锁隐性线粒体疾病,以心肌病、中性粒细胞减少、生长迟缓和3-甲基-戊二酸血症为特征。它是由TAZ突变引起的,已知TAZ突变编码tafazzin蛋白。DTNA编码a-肌营养不良蛋白,一种肌营养不良蛋白相关糖蛋白复合物。DTNA突变与LVNC相关。1同样,编码线粒体复合物Ⅱ催化成分琥珀酸脱氢酶复合物黄素蛋白亚基A(SDHA)的SDHA突变与新生儿心肌病相关。2尽管父亲的超声心动图显示疑似左心室致密化不全,但他没有心力衰竭临床证据。因此,DTNA和SDHA的突变可能不会导致严重的临床表型。
Discussion
This is the first report of LVNC due to triple mutation and associated with Barth syndrome. Barth syndrome is an X-linked recessive mitochondrial disorder characterized by car-diomyopathy, neutropenia, growth retardation, and 3-methyl-glutaconic aciduria. It is caused by mutations in TAZ, which is known to encode for the protein tafazzin. DTNA encodes for a-dystrobrevin, a member of the dystrophin-associated glycopro-tein complex. Mutations in DTNA are associated with LVNC.1 Similarly, mutations in SDHA encoding for succinate dehydro-genase complex flavoprotein subunit A (SDHA), the catalytic component of complex II of mitochondria, are associated with recessive neonatal isolated DCM.2 Although echocardiography of the father indicated suspected LVNC, he had no clinical evi-dence of heart failure. Therefore, the mutations in DTNA and SDHA may not result in a severe clinical phenotype.
Barth综合征可有更广泛的表型。由于家族在心脏病的发病年龄和严重程度上存在显著的变异性,因此,在巴特综合征的临床表现背后,可能有多重遗传因素。3 多突变肥厚型心肌病的表型比单突变更为严重。4 在心律失常发生率方面,室性心肌病可有多重突变/变异,可能导致表型表现增加。5在目前的Barth综合征患者中,尽管机制尚不清楚,但早期严重心力衰竭很可能是由多重突变引起的。
Barth syndrome has a much broader phenotype. Because the family had significant variability in the age of presentation and severity of the cardiac disease, additional genetic factors must be involved in the complete clinical expression of Barth syndrome.3 Hypertrophic cardiomyopathy with multiple mutations has a more severe phenotype than that with a single mutation.4 In arrhythmogenic right ventricular cardiomyopathy, the presence of an additional mutation/variation, such as a disease-causing one, may lead to increased phenotype manifestations.5 In the present patient with Barth syndrome, although the mechanism is unknown, the early-onset severe heart failure is likely to be caused by the multiple mutations.
References
1 Ichida F. Left ventricular noncompaction. Circ. J. 2009; 73: 19–26.
2 Levitas A, Muhammad E, Harel G et al. Familial neonatal isolated cardiomyopathy caused by a mutation in the flavoprotein subunit of succinate dehydrogenase. Eur. J. Hum. Genet. 2010; 18: 1160–5.
3 Ronvelia D, Greenwood J, Platt J, Hakim S, Zaragoza MV. Intrafamilial variability for novel TAZ gene mutation: Barth syndrome with dilated cardiomyopathy and heart failure in an infant and left ventricular noncompaction in his great-uncle.
Mol. Genet. Metab. 2012; 107: 428–32.
4 Ho CY, Lever HM, DeSanctis R, Farver CF, Seidman JG, Seidman CE. Homozygous mutation in cardiac troponin T: Implications for hypertrophic cardiomyopathy. Circulation 2000; 102: 1950–5.
5 Xu T, Yang Z, Vatta M et al. Compound and digenic heterozygosity contributes to arrhythmogenic right ventricular cardiomyopathy. J. Am. Coll. Cardiol. 2010; 55: 587–97.